Gastric Sleeve Diet - Dietary Guidelines for Gastric Sleeve Patients
Your diet will change with gastric sleeve surgery. Some changes are required to accommodate the smaller stomach size and some changes are necessary for weight loss and nutritional health.
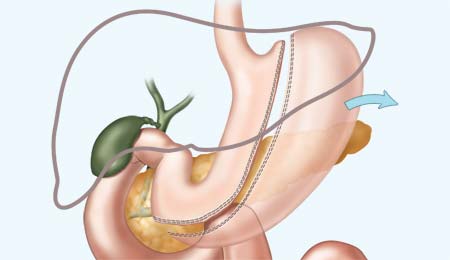
Gastric sleeve surgery
has fewer diet restrictions
compared to other procedures.
One of the benefits of the gastric sleeve is that there are fewer restrictions on the types of food patients can eat after surgery compared to other procedures. The surgery will force you to eat less at any one time, but it is up to you to choose healthy foods and limit daily caloric intake.
The following guidelines provide a general overview of what you can expect out of your eating experiences after surgery as well as helpful tips for achieving the best outcomes. Keep in mind that dietary advice can vary among surgeons and patients and you should follow the instructions given to you by your own bariatric team.

The gastric sleeve diet is designed to:
- maximize weight loss
- avoid gastric discomfort
- reduce the risk of complications and side effects
- prevent nutritional deficiencies
Preparing for Surgery
The last few weeks before surgery is the time to transition to a pre-op diet and make preparations for your recovery diet.
Pre-Op Diet: Before surgery, your surgeon will probably place you on a high-protein, liquid diet to help shrink your liver and make surgery safer. You will need to get a protein shake mixture that is low in sugars and carbohydrates and make protein shakes for one or more meals.
Pantry Preparation: Before surgery, go grocery shopping and stock up on the foods and supplies that you will need for your recovery. When you come home from surgery, you will need some time to recover and should already have the necessary items on hand for the first weeks of your post-op diet.
Items to purchase include: protein powder, clear broth and bouillon, non-fat milk, decaf tea and coffee (artificial sweeteners and non-dairy creamer), sugar-free Jello, sugar-free popsicles, sugar-free drinks, sugar-free instant breakfast, supplements, medications.
Recovering from Surgery
The diet will gradually progress from liquids to solid foods as your body recovers from surgery and you adapt to eating with the gastric sleeve. Your doctor will monitor your recovery and let you know when it is safe to advance through the stages and add foods to the diet.

Recovery Diet Progression
- Stage 1: Clear to Full Liquids
- Stage 2: Pureed Foods
- Stage 3: Soft Foods
- Stage 4: Solid Foods
Stage 1: Clear to Full Liquids
This stage includes sugar-free and non-carbonated liquids, progressing from clear liquids to full liquids. Take small sips throughout the day and pay attention to the feeling of fullness.
Clear liquids are items such as soup broth or bouillon, fruit juice (grape, apple and cranberry; avoid citrus or tomato), Crystal Light or sugar-free Kool-Aid, decaf coffee or tea, herbal tea, Jello, sugar-free fruit ices and popsicles, sugar-free sherbert, sugar-free Carnation instant breakfast, water, sugar-free flavored non-carbonated waters.
Full liquids are items such as non-fat milk, low-fat creamed soups (diluted and no chunks), cooked and blended cereals (cream of wheat, oatmeal), natural applesauce, non-fat/sugar-free yogurt (no chunks), sugar-free pudding.
Stage 2: Pureed Foods
Once you tolerate liquids, you will be able to start on pureed foods. It may only take a few days to advance from liquids to pureed foods, but this stage can last weeks. Pureed foods should have the consistency of applesauce and include a variety of foods that have been blended to a thin and smooth texture.
- Examples of pureed foods are blenderized fruit, blenderized meat, blenderized soups, blenderized beans, mashed potatoes, scrambled eggs, hummus, soft-canned fruits, soft-cooked vegetables, cottage cheese, refried beans with melted cheese. You may use non-spicy herbs and seasonings to flavor the food.
Meals will start out small and frequent (about 1/4 cup, 6 times a day). Eventually you will be able to eat a little more food at meals (about 1/2 cup, 4 to 6 times a day). Eat slowly (30 minutes for a 1/2 cup meal). Drink plenty of fluids (about 8 cups) throughout the day to avoid dehydration, but not within 30 -45 minutes of a meal.
Stage 3: Soft Foods
After pureed foods are well tolerated and healing has progressed, you will be able to start adding soft foods to the diet. This is generally sometime around 4 weeks after surgery. New foods should be added to the diet one at a time to observe your reaction to it.
- Soft foods include items such as hot cereals with skim milk, light yogurt, cooked eggs (not fried), chopped or canned lean meat (fish, tuna fish, chicken, turkey), cooked vegetables (peeled), beans and legumes, softened cold cereal (without sugar), canned fruits, casseroles (such as macaroni and cheese or tuna), toasted bread, crackers, or pretzels.
Make sure meal sizes are small (about 3/4 cup), eat slowly (about 1/2 hour), take small bites and chew food thoroughly. Liquids should typically not be consumed with foods, but if needed, it is okay to take a few small sips of liquid with your meals. Continue to drink plenty of liquids between meals.

Stage 4: Solid Foods - Diet After Recovery
Your surgeon and dietician will let you know when you can start to eat solid foods. It will take some time to get to this stage, often not until about 3 months after surgery.
The gastric sleeve will allow you to eat almost any type or texture of food, provided you limit portion sizes, eat slowly, and chew food thoroughly. You will eventually be able to try red meat, vegetables and fruits with skins, and even whole grain bread.
Tips for the best results:
Make sure to follow the eating and drinking instructions of your bariatric surgeon and wait for approval before adding foods to the diet. If you add foods too soon or eat foods you have been told to avoid, you could damage your stomach or experience uncomfortable side effects such as nausea, stomach cramps, and vomiting.
New foods should be added one at a time to identify your tolerance for specific food items.
High protein levels
are needed in the diet
to keep the body from
using muscle tissue
for energy instead
of excess fat when on
a low-calorie diet.
Eat foods that provide your body with nutrients. Your diet is limited in quantity so it is important to make every calorie count. Your diet should focus on protein rich foods (non-fat or 1% milk products, egg whites, low-fat cheese, fish, chicken, turkey, pork tenderloin, extra-lean ground beef, soy products) supplemented by fruits, vegetables, and whole grains.
Drink plenty of liquids (8 cups daily) to stay hydrated. Sip throughout the day but avoid drinking within 30-45 minutes of a meal. Do not use straws as it can contribute to gas.
Do not drink your calories. Choose beverages that are low-calorie, sugar-free and non-carbonated. Avoid soda (gases stretch stomach pouch) and alcohol (high in calories).
Take your vitamin and mineral supplements. They must be taken regularly for life to ensure you are getting enough of the necessary nutrients to maintain good health.
Keep a food journal of what you eat, how much you eat, and how the food is prepared. This will help you track calories, measure protein intake, and identify your reactions to new foods.
Keep your scheduled follow-up appointments with your surgeon and dietician. This is the time to evaluate your progress and discuss your diet plan.
Try new recipes and eat a wide variety of nutritious foods. You may be eating less, but you can still find foods that you enjoy eating.
Diet Q & A
Q: Why is protein a priority in the diet?
A: Dietary protein is vital for health and life. The body needs adequate protein for cells and tissues to function properly, to help with wound healing, minimize hair loss, preserve lean muscle mass, and enhance fat-burning metabolism.
Q: Why shouldn't I drink carbonated beverages?
A: Many gastric sleeve patients are advised to avoid drinking carbonated beverages. This is because carbonation can cause bloating and discomfort, especially with the smaller stomach pouch and slower digestion after gastric sleeve surgery. Also, some seltzer waters and diet sodas contain acids and salts due to the sodium, potassium, and phosphorus. Drinking them can negatively affect the balance of minerals in the body and prevent the absorption of calcium, causing harm to the bones.
Q: Why have I been told not to drink from a straw?
A: Drinking from a straw is one of the eating behaviors that gastric sleeve patients are told to avoid as it may allow too much air into the stomach and cause bloating and discomfort.
Q: Why should I avoid caffeinated beverages?
A: Most bariatric surgeons advise their gastric sleeve patients to avoid caffeinated beverages. One of the primary concerns is that caffeine is one of the known substances that promotes gastric acid production and gastroesophageal reflux. Other concerns are that it can interfere with nutrient absorption, increase hunger, and increase risk of dehydration.
Nutrition & Diet Resources
Learn more about healthy food groups at ChooseMyPlate.gov.
Related Articles
Social
Eat Healthy!
Eating healthy requires choosing the right types of food as well as controlling the amount of food that is eaten. Read the Nutritional Facts label on packaged foods to find out serving size, calories, and nutrient information.