Duodenal Switch Bariatric Surgery
The duodenal switch is a very effective type of bariatric surgery with great weight loss potential. The procedure can help patients lose a substantial amount of excess weight as well as maintain successful weight loss over time. The duodenal switch weight loss procedure moderately restricts food consumption, but it primarily promotes weight loss through malabsorption.
The Duodenal Switch procedure
assists with weight loss
by reducing food absorption.
The duodenal switch is not as common as gastric bypass or lap band surgery, but it is gaining more attention as an alternative to gastric bypass for individuals with a BMI greater than 50. The procedure is complex and may not be the right approach for every bariatric patient, but for some individuals it offers many advantages. It is often the preferred option for individuals with very severe obesity.
If you are looking into your bariatric options, the following information can provide you with an overview of duodenal switch weight loss surgery, including a surgical overview, the advantages and disadvantages of the procedure, patient criteria, and expected weight loss results.
About the Procedure
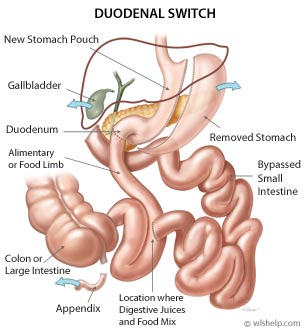
The duodenal switch (DS), also known as the biliopancreatic diversion with duodenal switch (BPD-DS), or the vertical gastrectomy with duodenal switch, was developed in the late 1980's as a variation of the biliopancreatic diversion weight loss procedure. The changes reduced the incidence of stomal ulcer, dumping syndrome, and serious protein-calorie malnutrition.
How the duodenal switch procedure works:
- Restricts the amount of food that can be eaten by reducing the size of the stomach by 60 to 80% (vertical gastrectomy)
- Limits the amount of food that is absorbed by the body due to rerouting the small intestine so that food bypasses a large portion of the digestive tract (duodenal switch)
The duodenal switch weight loss surgery combines two separate procedures, the vertical gastrectomy (stomach removal) and the duodenal switch (intestinal bypass), to assist with weight loss.
The duodenal switch procedure is a surgically complex type of weight loss surgery. It is a more difficult operation to learn compared to Roux-en-Y gastric bypass or lap band surgery and is performed by very few surgeons worldwide. Also, some surgeons do not perform the surgery because of concerns about the long term effects of malabsorption.

Restrictive Weight Loss Component
The vertical gastrectomy procedure reduces the size of the stomach to limit food consumption, although not to the degree of gastric bypass surgery or adjustable gastric banding. This allows duodenal patients to eat more normal sized meals than other bariatric patients.
During surgery, the left side of the stomach is permanently removed, creating a narrow, crescent shaped stomach that extends from the esophagus to the small intestine. The pylorus (stomach outlet valve) is kept intact to regulate movement of food to the intestines, avoiding the incidence of dumping syndrome common with gastric bypass surgery.
Malabsorptive Weight Loss Component
The malabsorptive aspect of duodenal switch is very successful in promoting weight loss, but the unknown long-term nutritional effects and associated possible complications of malabsorption make the duodenal switch more controversial than other weight loss procedures. Following duodenal switch surgery, patients require lifelong monitoring and nutritional supplements to avoid nutritional deficiencies.
During surgery, the small intestine is divided and rearranged to separate food from the digestive juices for most of the length of the intestines. This prevents the body from absorbing all of the calories consumed. The middle portion of the small intestine is cut out in order to reduce the length of the food limb. The cuts are made just past the stomach outlet at the beginning and about eight feet from the lower end of the small intestine, creating a shorter food limb. The cut end of the food limb is then attached to the duodenum (top portion of the small intestine) to transport food from the stomach to the colon. The divided middle portion of the small intestine remains connected to the liver and pancreas at the beginning section while the lower end is reconnected to the last section of the small intestine. It moves the digestive juices separately from the food until they are rejoined in the last section of the small intestine, where they travel together in the common limb for a short distance.
Duodenal Switch Patient Criteria
The duodenal switchprocedure is often
the preferred option
for patients with
a body mass index
greater than 50.
Individuals who may be a good candidate for duodenal switch surgery are those with a body mass index greater than 40 and between the ages of 18 and 65. For patients with a body mass index greater than 50, the duodenal switch is often the preferred bariatric surgery procedure. Individuals interested in the duodenal switch weight loss surgery should discuss this procedure with his or her bariatric surgeon to determine whether or not it is an appropriate option to pursue.
Duodenal Switch Advantages
- Patients are able to eat more normal sized meals than other bariatric patients, resulting in a higher level of patient satisfaction
- The hunger hormone, Ghrelin, is greatly reduced due to removing a large section of the stomach
- Pyloric valve is kept intact, avoiding the incidence of dumping syndrome and stomal ulcers that occur with gastric bypass surgery
- Very effective weight loss method for patients with BMI greater than 50
- Super obese patients who are turned down for other types of bariatric surgery may qualify for the DS procedure
- Patients are able to achieve significant and long-lasting weight loss due to the malabsorptive component of the procedure
- Average weight loss of 60-80% excess weight
Duodenal Switch Disadvantages
- Lifelong nutritional supplementation is required, otherwise health problems can occur
- Lifelong monitoring for nutritional deficiencies, including protein malnutrition, anemia and bone disease
- Some foods may cause intestinal irritation, gas pains, bloating, frequent passing of very smelly gas
- May develop intolerance of certain foods (varies by patient)
- May cause changes in body odor
- Often considered investigational by insurance companies and may not be a covered procedure
- Complex procedure, performed by very few bariatric surgeons
Duodenal Switch Results
Follow-up studies show that most duodenal switch patients are able to tolerate the procedure well and are quite satisfied with the weight loss results. On average, DS patients lose about 60 to 80% of their excess body weight and experience minimal weight regain. Also, DS patients show an improvement or resolution of many obesity comorbidities, including type 2 diabetes and high blood pressure. Overall, the duodenal switch weight loss surgery has helped many seriously obese patients greatly improve their overall health and quality of life.
Related Articles
Social
Compare!
Each bariatric surgery procedure has its own advantages and disadvantages. Don't choose a procedure based on what is popular at the moment, rather compare the options and decide which one is right for you.




